
SCDAC/AAFC
Unit 34,
260 Adelaide St. E,
Toronto, ON M5A 1N1.
Canada
© All rights reserved The Sickle Cell Disease Association of Canada/L’Association D’Anémie Falciforme Du Canada (SCDAC/AAFC)
Hemoglobin disorders such as sickle cell disease and thalassemia are the most common genetic diseases in the world. Three hundred thousand (300,000) babies are born each year with sickle cell disease, and millions of individuals are affected worldwide. Epidemiological models predict that these numbers could increase by at least 25% to 400,000 babies with sickle cell disease per year by 2050. Recognizing sickle cell disease as a global health problem, the World Health Organization adopted two resolutions in 2006 and 2010, calling on countries to strengthen their responses to the disease.
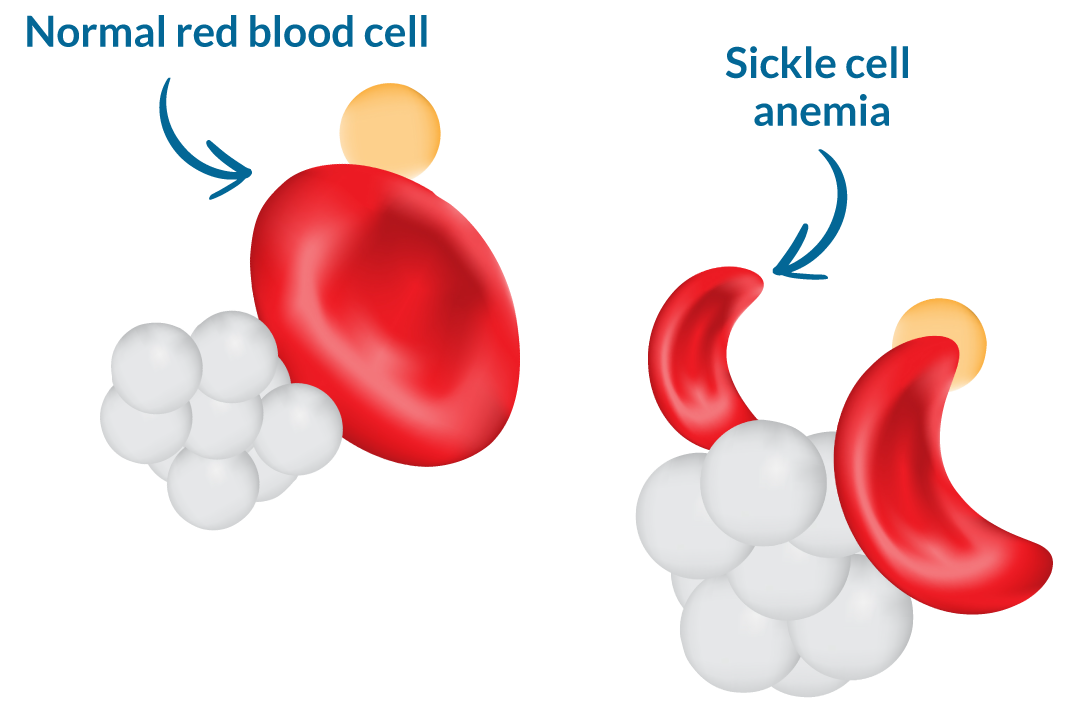
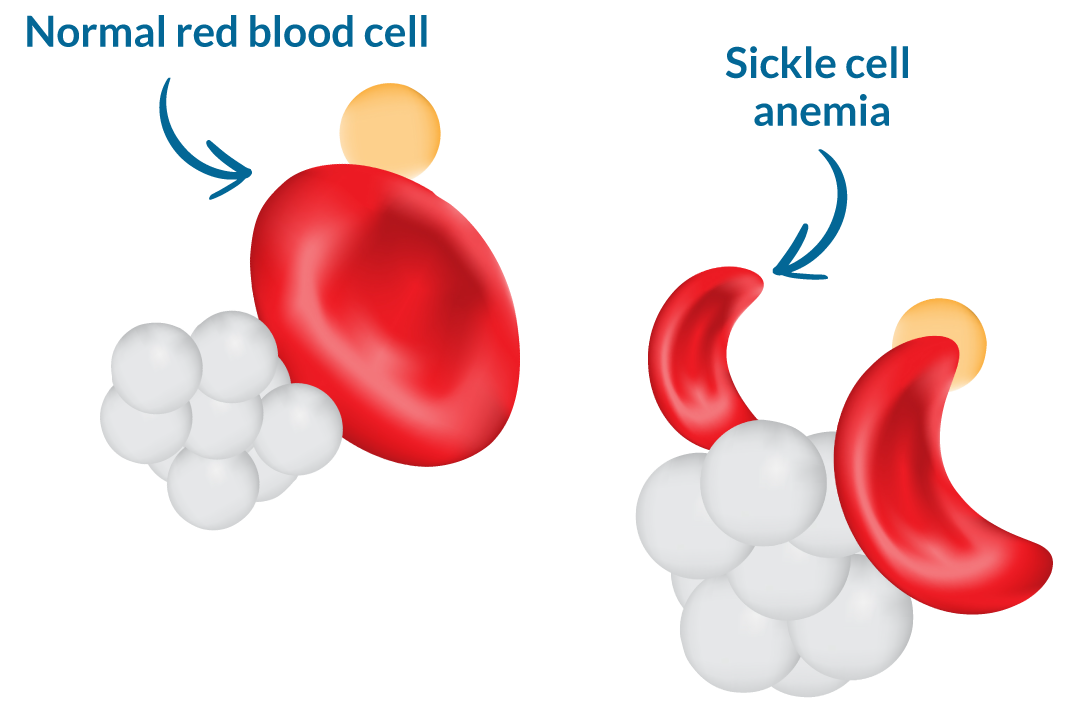
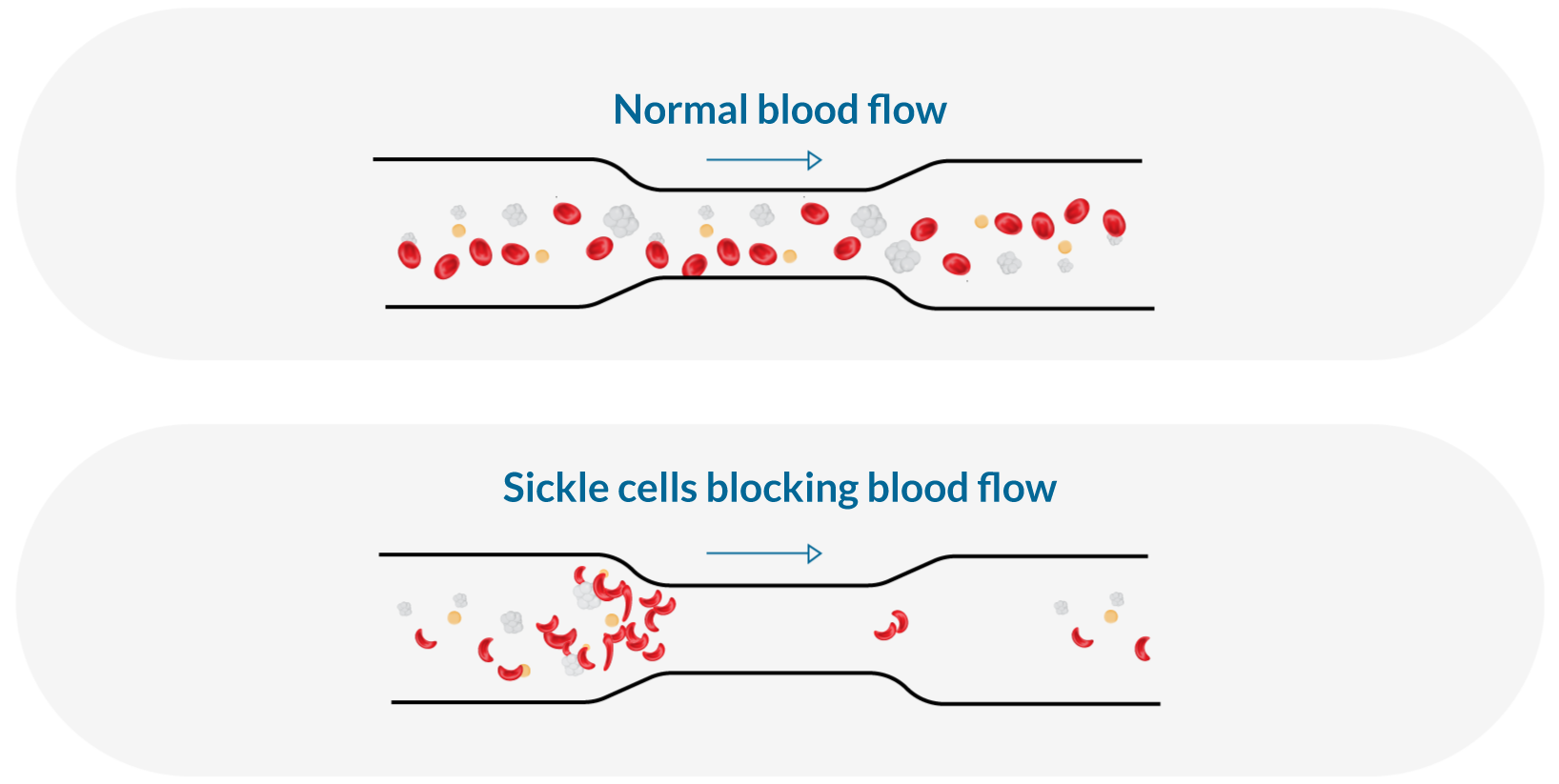
Sickle cell anemia or sickle cell disease is considered a serious blood disease. The red blood cells of patients with sickle cell disease are deformed under hypoxic conditions. Sickle cell disease can disrupt normal blood flow, leading to occlusion of blood vessels and tissue damage due to ischemia-reperfusion lesions. Sickle cell disease therefore has devastating consequences on quality of life and health. Manifestations of the disease include episodes of severe pain, an increased risk of serious infection and death, a risk of stroke up to 300 times higher than that of normal individuals, and damage to almost all organs. People with this disease are also at increased risk of sudden death and have a reduced life expectancy.
Sickle cell anemia or sickle cell disease is a genetic condition that causes red blood cells to deform. As it is these globules that transport oxygen in the body, their deficiency leads to multiple complications. The condition or disease is hereditary because it is transmitted by both parents when they are carriers of the gene.
Are there different types of sickle cell disease?
There are three types of sickle cell anemia commonly diagnosed:
– Hemoglobin SS or sickle cell disease
– Hemoglobin SC
– Hemoglobin of thalassemia beta
Each of these types can cause episodes of pain and complications, but some are more common than others. All of these types can also cause an increase in hemoglobin in the fetus, which can protect the red blood cells from sickle cell defects and help prevent complications.
What are those complications?
– Episodes of pain or vaso-occlusive crisis
– Strokes and strokes
– Lung infections or acute thoracic syndrome
– Leg ulcers (skin ulceration in lower leg)
– Bone injury or necrosis
– Yellow eyes or jaundice
– Early Gallstones
– pulmonary hypertension
– Kidney damage and loss of body water in urine
– Painful Erections in Humans (Priapism)
– Blockage of blood vessels in spleen or liver (splenic sequestration)
– Damage to the eyes
– Low red blood cell levels in the blood (anemia)
– Slowing growth
How can we help prevent these complications?
Anyone with sickle cell disease should be treated by a medical team that understands the disease. All newborns diagnosed with sickle cell anemia should receive penicillin daily and should be monitored closely to prevent serious infections and maintain their well-being. They should be given all childhood immunizations and a pneumococcal vaccine. Parents should know how to detect fever as this may signal the need for early medical attention for serious infection.
The following are general guidelines for maintaining the health of the patient with sickle cell anemia :
– Take folic acid (folate) daily to help produce new red blood cells
– Taking penicillin daily until age 6 to prevent serious infections
– Drink plenty of water every day (8-10 glasses for adults)
– Avoid temperature extremes, too hot or too cold
– Avoid overwork and stress
– Give yourself lots of rest
– Get regular follow-up from doctors who know this disease
Patients and their families should be alert to the following symptoms that require urgent medical evaluation :
– Take folic acid (folate) daily to help produce new red blood cells
– Taking penicillin daily until age 6 to prevent serious infections
– Drink plenty of water every day (8-10 glasses for adults)
– Avoid temperature extremes, too hot or too cold
– Avoid overwork and stress
– Give yourself lots of rest
– Get regular follow-up from doctors who know this disease
Recognition: Some information on this page is courtesy of:
Hemoglobin disorders such as sickle cell disease and thalassemia are the most common genetic diseases in the world. Three hundred thousand (300,000) babies are born each year with sickle cell disease, and millions of individuals are affected worldwide. Epidemiological models predict that these numbers could increase by at least 25% to 400,000 babies with sickle cell disease per year by 2050. Recognizing sickle cell disease as a global health problem, the World Health Organization adopted two resolutions in 2006 and 2010, calling on countries to strengthen their responses to the disease.
In Canada:
An estimated 6,000 Canadians are living with sickle cell disease.
About 1 in 2500 newborns in Canada will have sickle cell disease.
How can I meet a genetic counselor?
If you and your partner are carriers of sickle cell anemia, the genetic counselor will be able to tell you about the genetics of this disease and present you with the testing options available to you during pregnancy.
There is no treatment for sickle cell disease during pregnancy, but there are tests that can help find out as early as possible if the baby has sickle cell disease. Ask your doctor for a referral to your local genetic clinic. If you do not have a doctor, contact your local genetic clinic directly for more information.
Should we have our other children tested to see if they have sickle cell disease?
If only one parent carries sickle cell disease, there is a 1 in 2 (50%) chance that their other children carry sickle cell disease. Sickle cell testing is not usually done in childhood, since being a carrier does not cause health problems in childhood. The carrier test can be done with your other children when they are old enough to understand the information and decide for themselves if they wish to be tested. Some parents have their children tested at an earlier age and share this information later with the child, at a time they consider more appropriate for both their child and their family. If you have any questions about the test with your other children, talk to your doctor.
If both parents are carriers, it would be better to have your other children tested.
Should my loved ones be screened for sickle cell disease trait?
Other family members (e.g., cousins, aunts, uncles) may be carriers of sickle cell disease. It is important to inform family members of this risk. They can decide whether or not to be tested for sickle cell disease. This is especially significant if they are planning to have children. Sometimes family members have the disease.
Newborn screening
The provinces of Ontario, British Columbia, Nova Scotia, New Brunswick, Prince Edward Island, Yukon, Alberta, and the Northwest Territories, and progressively Quebec have included sickle cell disease in their newborn screening programs. Only two provinces and one territory remain before the goal of universal newborn screening for sickle cell disease is achieved across Canada.
We will continue to advocate for other provinces and territories to include universal screening for sickle cell disease.
Screening is simply a blood test at birth to detect the presence of sickle cell anemia or the sickle cell trait.The variants targeted in screening are: HbSS, HbSC, HbSβ-thalassemia, HbSOarab and HbSDpunjab.
What does it mean to have sickle cell trait?
The sickle cell trait means that the person carries a gene that produces sickle cell hemoglobin, inherited from his or her parents, and a gene for normal hemoglobin. Normal hemoglobin is called type A and sickle cell hemoglobin is called type S. The sickle cell trait means the presence of AS hemoglobin on hemoglobin electrophoresis. This does NOT cause sickle cell disease.
In Quebec, sickle cell carrier status results are only available upon request.
The Sickle Cell Association of Canada and its members continue to raise awareness of this debilitating disease. This legislation has resulted in increased awareness and education regarding Sickle Cell Anemia, resulting in a more informed medical staff and improved standardized access to integrated care.
Providing expectant parents with relevant information and appropriate support so that they can make informed decisions before starting a family will reduce the number of births of children with Sickle cell disease, She spares many patients and their families from a Lifetime of pain and hardship related to this disease. Increased awareness also stimulates interest in scientific medical research on Sickle cell disease.
Our awareness campaign will help people with AIDS make healthy lifestyle choices to live better lives. Join us as a partner in our efforts to raise awareness and educate people about sickle cell disease.
To raise awareness of sickle cell disease, SCDAC has developed bracelets and T-shirts to raise awareness. We also encourage you to participate in our efforts to raise awareness of this disease.
As a patient:
– Learn about sickle cell disease and its treatment
– Contact a hematologist for full treatment of sickle cell anemia
– Contact your local sickle cell disease association
– Join a local patient support group
As a friend or relative:
– Understand that individuals and families affected by sickle cell disease need support
– Keep in touch and offer assistance where possible
– Offer childcare or other services where possible
– Donate blood
In schools:
– Organize awareness days, possibly June 19 or in September, to inform teachers, staff and students
– Implement accommodations for students who are absent due to illness
As a healthcare professional:
– Learn more about Sickle Cell Disease
– Keep brochures on the disease and the trait of sickle cell anemia from the SCDAC in your office
– Add sickle cell disease and trait information to the patient history form
– Refer individuals with the sickle cell trait to a genetic counselor
– Familiarize yourself with the protocol for treating a sickle cell crisis
how to become
a Life Partner, donate blood
and save lives
how to become
a Life Partner, donate blood
and save lives
Step 1
Become a Life Partner
Step 2
Make an appointment at a center to donate:
Blood Donation Information :
The Sickle Cell Association of Canada and regional groups have Partner for Life numbers with Canadian Blood Services.
Here’s how to become a Life Partner, donate blood and save lives. It’s a simple, five-step process:
1. Create an account at blood.ca/pfl or on the GiveBlood app for Apple or Android.
2. Select “Partners” from the menu
3. Select “join a team” and type Sickle Cell Disease Association of Canada in the search bar.
Partners for Life PLV IDs are used to link people’s donations to organizations that are important to them.
Members of your network will need your PLV ID number when they register online at blood.ca to have their blood donations count towards your organization’s pledge.
Registration is a one-time process and people can choose to “opt out” of the team at any time through their donor account.
You can reach the AAFC National Team with the national number: SICK0090755
Or use a number in your area to donate blood:
Alberta: SICK0090807
Ontario: SICK0091321
British Columbia: SICK0090763
Manitoba: SICK0090738
Atlantic Canada (Nova Scotia, Newfoundland and Labrador, New Brunswick and Prince Edward Island): SICK0091321
Saskatchewan: SICK0090934
Share your donation experience with us, tag us on social media.
@SICKLE CELL DISEASE